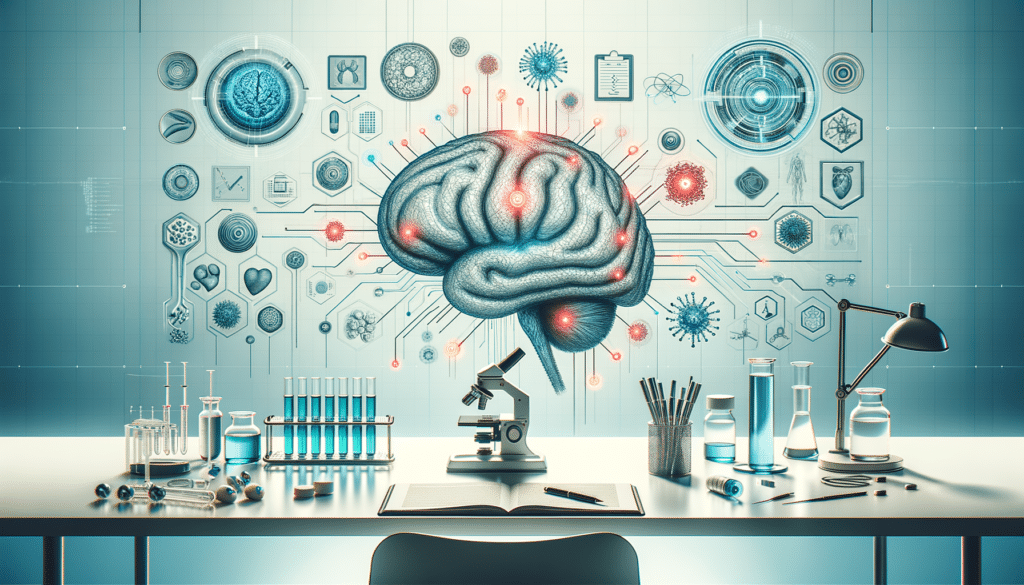
Understanding Parkinson’s Disease: A Brief Overview
Parkinson’s Disease (PD) is a progressive neurological disorder that primarily affects movement. It is characterized by tremors, stiffness, slowness of movement, and impaired balance. The disease results from the degeneration of dopamine-producing neurons in the brain, particularly in the substantia nigra. Although the exact cause of Parkinson’s remains unknown, research suggests a combination of genetic and environmental factors. Understanding the underlying mechanisms of PD is crucial for developing effective treatments and management strategies.
Parkinson’s affects millions worldwide, with a higher prevalence in older populations. Symptoms typically begin subtly and progress over time, making early diagnosis challenging yet essential for effective management. While there is currently no cure for Parkinson’s, a variety of treatments are available to manage symptoms and improve quality of life. These treatments often involve a combination of medication, lifestyle changes, and supportive therapies.
Medications: The Cornerstone of Parkinson’s Management
Medications play a pivotal role in managing Parkinson’s Disease, primarily by addressing dopamine deficiency in the brain. The most widely used medication is Levodopa, which converts into dopamine in the brain, helping to alleviate symptoms like tremors and rigidity. Often combined with Carbidopa to prevent premature conversion outside the brain, this treatment remains one of the top options for symptom management.
Other medications include dopamine agonists, which mimic dopamine effects, and MAO-B inhibitors, which prevent dopamine breakdown. Each medication has its benefits and potential side effects, requiring careful selection and monitoring by healthcare professionals. Tailoring medication plans to individual needs is crucial, as each patient may respond differently to treatments.
Key considerations in medication management include:
- Timing: Consistent medication schedules are vital to maintain symptom control.
- Side Effects: Monitoring and managing side effects, such as nausea or dizziness, is essential.
- Adjustments: Regular assessments to adjust dosages or switch medications as the disease progresses.
Integrative Therapies and Lifestyle Modifications
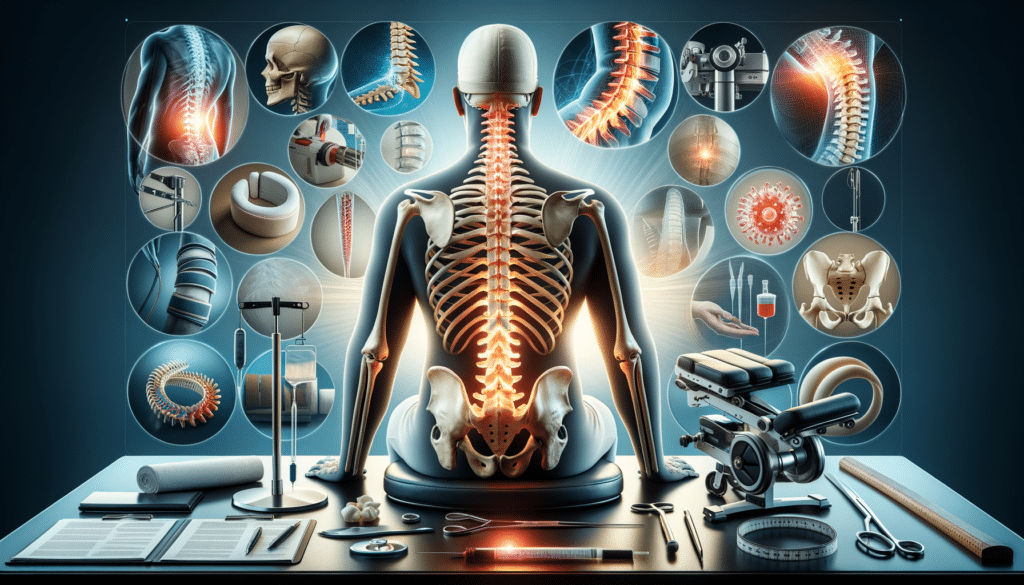
Beyond medication, integrative therapies and lifestyle modifications are essential components of Parkinson’s management. Physical therapy can enhance mobility and balance, reducing the risk of falls. Occupational therapy helps individuals maintain independence by adapting daily activities and environments to their needs.
Exercise is particularly beneficial, with activities like tai chi, yoga, and strength training improving flexibility, strength, and overall well-being. Regular physical activity has been shown to slow the progression of symptoms and enhance quality of life. Nutrition also plays a role, with a balanced diet supporting overall health and potentially mitigating some symptoms.
Support groups and counseling provide emotional and psychological support, helping individuals and families navigate the challenges of living with Parkinson’s. These resources offer a sense of community and shared experiences, which can be invaluable in managing the emotional impact of the disease.
In summary, managing Parkinson’s Disease requires a comprehensive approach that combines medication, integrative therapies, and lifestyle changes. By tailoring treatments to individual needs and focusing on holistic care, individuals with Parkinson’s can lead fulfilling lives despite the challenges of the condition.